But Forensic Patients Filling State Hospitals
Virginia’s mental health crisis services system has itself been in crisis for years, with overcrowded state hospitals, staff vacancies and waits for crisis care in emergency rooms lasting days, not hours. Virginia’s Behavioral Health Commission recently heard a report from the Commissioner of Behavioral Health about good progress in beginning to turn the system around. This is great news.
Significant funding and an intensive “Right Help, Right Now” transformation strategy is beginning to divert more individuals in crisis from civil hospital commitment, through local Community Services Boards, the 988 crisis call system, new mobile crisis response teams and new community treatment facilities. According to the Department of Behavioral Health & Developmental Services (DBHDS), there are now 98 mobile crisis teams across the state, with a goal of 140. There are now 264 beds in local receiving centers and stabilization units, with another 287 under development.
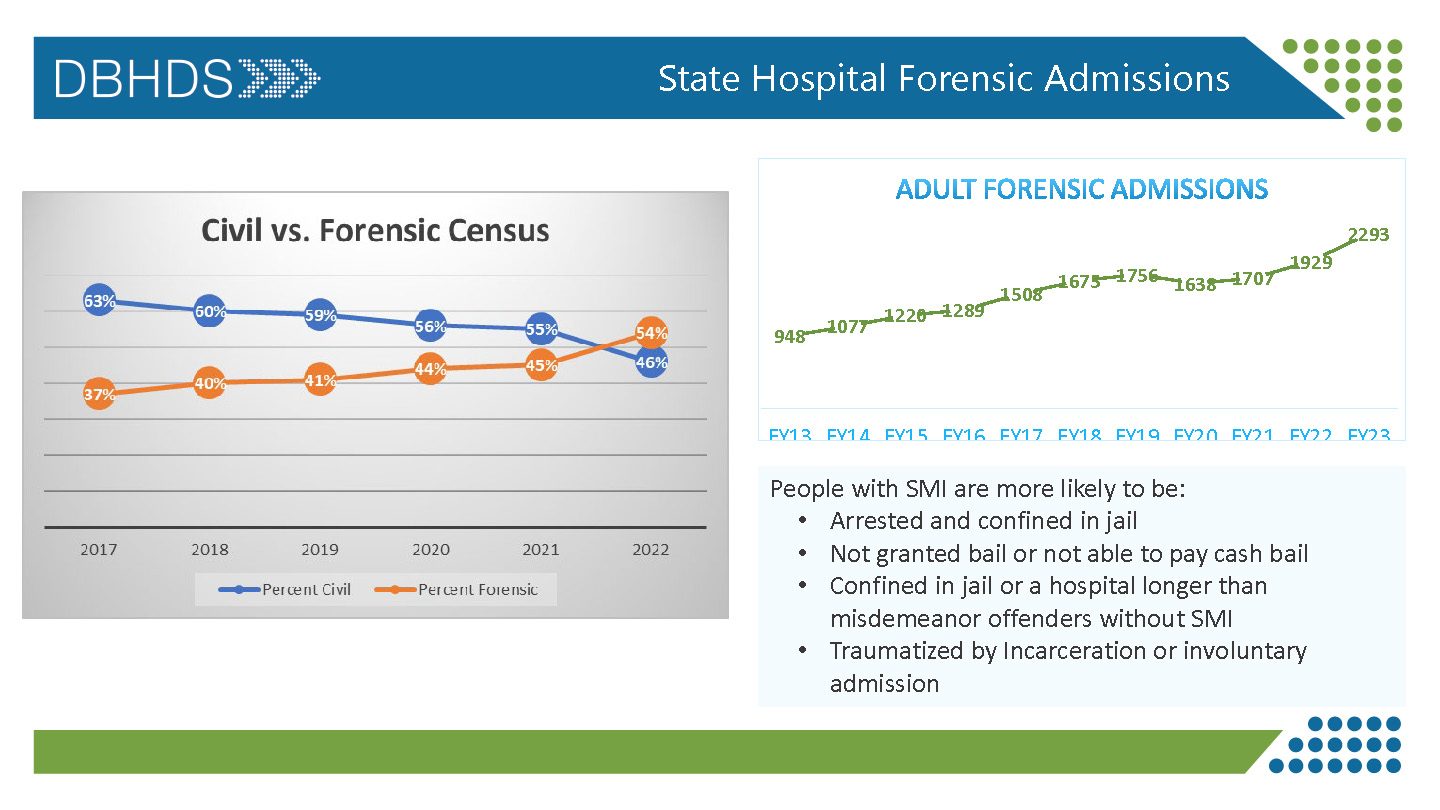
All of the above efforts are helping provide people appropriate crisis care in their own communities and reducing our overreliance on the state hospital system, thus freeing up beds for longer term care. However, state psychiatric hospitals remain full due to increased forensic admissions.
Around 92% of Eastern State Hospital beds and 87% of Central State beds are currently occupied by forensic patients, or individuals coming through the criminal justice system. Most of the increase is for orders to restore an individual’s competency to stand trial, which increased 143% since 2014.
Restoration includes medications and programs with a goal only to help defendants be able to understand their charges and the process so they can assist their lawyer with their own defense. Patients stay an average of 106 days in the hospital, and when restored are returned to jail. Around 30% of restoration admissions are for misdemeanor offenses, and when returned to jail they often get released on time served.
Jail Discharge Planning Could Help
Changing the competency restoration process is complicated, and ultimately it depends on a better mental health system and resources at all levels, including prevention, crisis, treatment and recovery services. But there are many approaches that could help, including working with courts to provide for restoration at the community level.
Recognizing that many defendants with a serious mental illness have been in jail before, often for misdemeanors, better planning prior to their release from incarceration can connect them with community treatment, peer support, safe housing and other resources to help them stay out of the criminal justice system.
Less than 30% of local and regional jails have discharge planning services for individuals with a mental illness, despite plans from seven years ago to implement them statewide. The service can make a big difference in connecting individuals successfully into the community following incarceration.
Legislation passed in 2017 charged DBHDS with convening a workgroup to develop a comprehensive plan to address the needs of this population as they are released from jail. The workgroup report (Forensic Discharge Planning for Persons with Serious Mental Illness in Virginia Jails) https://rga.lis.virginia.gov/Published/2017/RD470 recommended a phased implementation to provide discharge planner services to all jails.
Today, DBHDS funds 13 Forensic Discharge Planning programs with a total of $3,700,800 in annual funding. These programs include 22 Community Services Boards in 21 Local & Regional Jails. Good progress, but a long way from full implementation in 70 jail facilities.
In addition, for five years the Department of Criminal Justice Services has run a “pilot” program to fund mental health services in six local jails (now five jails since Hampton Roads Regional Jail has closed): Chesterfield County Jail, Middle River Regional Jail, Western Virginia Regional Jail, Richmond City Jail, and Prince William Adult Detention Center. There is $2 million/year to continue the pilot programs authorized in Item 398, Chapter 836, 2017 Acts of Assembly. The budget language will not allow expansion. Their focus appears to be on services within the jail, although they are to include “provision of appropriate services after release.” If these services are working, the legislature should have expanded them by now.
A related, but more involved step is to find out which jails have fully implemented mental health services in compliance with the Minimum Standards for Behavioral Healthcare in jails. The Compensation Board has funded many new positions, but we don’t know the results. And the number of people with a serious mental illness in our local jails is growing.
A serious mental illness doesn’t have to result in arrest and incarceration, whether the time is served in a local jail or a state hospital. In conjunction with transforming crisis services, we need more diversion programs to keep people out of the criminal justice system, and more services for those within it.