The following is a guest post. Opinions expressed in this post are the author’s own.
Virginia’s recent legislative session produced several bills and budget amendments to improve mental health services. However, Virginia Governor Terry McAuliffe challenged state legislators to also include jail mental health assessments and investigation of certain jail deaths in Virginia’s budget. The legislature’s actions and Governor McAuliffe’s concerns highlight the tremendous impact funding concerns have on mental health services for the general population and for jail-prison populations. Previous budget cuts and funding concerns have increased already existing program constraints at local, state, and national levels.
Over the years organizations have conducted research to further understand mental illness and incarceration. In 2014, The Treatment Advocacy Center did a survey for every state, Virginia is on page 93, to examine how common it is for people with mental illness to be incarcerated (also known as “mental illness-to-incarceration-pipeline”). As with budget cuts and funding concerns, the incarceration of people with mental illness is prevalent locally, statewide, and nationwide. There is substantial impact on people of lower socioeconomic status and blacks and non-white Hispanics.
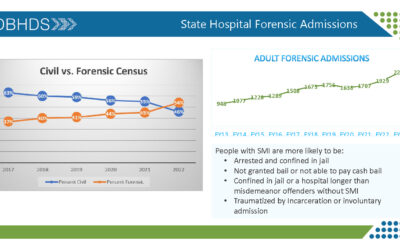
To further capture the pattern of mental illness-to-incarceration, the 2016 Mental Illness in Jails Report found 6,554 jail inmates (almost 49% pre-trial; 51% post-conviction) are known to have or are suspected to have a mental illness. Of approximately 39,888 inmates in the general inmate population in 2016, there are approximately 16% with mental illness and 8% with serious mental illness (schizophrenia/delusional, PTSD, bipolar/major depressive).
Existing programs that provide mental health services to incarcerated populations include Virginia Department of Corrections Mental Health Services; and provide training to law enforcement representatives to further encourage crisis de-escalation include the Virginia Crisis Intervention Team Coalition. The mental health Crisis Intervention Team concept started in Memphis, Tennessee and has spread nationally and internationally. We need more collaborations with mental health organizations, law enforcement, and communities. Increased collaborations potentially increase access to mental health services, reduce forms of violence and crime, and decrease incarceration of people with mental illness.
Challenging the “mental illness-to-jail/prison-pipeline” includes under-served populations in Virginia: Individuals, families, and communities in which mental health is silenced and shamed. This includes, but is not limited to, gender; race, ethnicity, and culture; LGBTQ; and cultural and societal barriers. There are Virginians with less access to mental health services because of geography, cost, or cultural beliefs. Some people’s identity is shamed by other people (e.g., LGBTQ) and they are unable to talk to family, friends, and community members about their identity, let alone mental health issues. There can also be difficulty finding local mental health services that match people’s school and work schedules, can be reached through public transportation, and are affordable since most people lack private insurance or employment insurance. This can increase the prevalence of mental struggles, violence, and being placed in the criminal justice system.
Therefore, we need to examine factors that contribute to access to and under-use of mental health services: Under-served populations; correlation between mental illness, violence, and crime; and the mental illness-to-incarceration-pipeline. To capture this we must continue to challenge the dehumanization of people in jails and prisons. We must also continue to highlight how such challenges need funding. Yes, there are Virginia families and Virginia professionals passionate about this issue. Yes, there are Virginia families and Virginia professionals that will keep working despite funding concerns. However, we should not be met with minimal resources. We need resources to provide resources.
By Kimya N. Dennis
 Kimya N. Dennis is a sociologist and criminologist originally from Richmond, VA. She lives in Winston-Salem, NC and does interdisciplinary work on mental health, suicide and suicidal self-harm, and reproductive choices. Dr. Dennis’s work reaches diverse audiences and particularly under-served populations. She is on the board of directors for The Mental Health Association in Forsyth County, North Carolina chapter of American Foundation for Suicide Prevention, and LEAD Girls of NC. Dr. Dennis is faculty and the creator and Coordinator of the Criminal Studies program in the Department of Sociology and Criminal Studies at Salem College in Winston-Salem, NC. She can be contacted: www.kimyandennis.com ; kimya@kimyandennis.com
Kimya N. Dennis is a sociologist and criminologist originally from Richmond, VA. She lives in Winston-Salem, NC and does interdisciplinary work on mental health, suicide and suicidal self-harm, and reproductive choices. Dr. Dennis’s work reaches diverse audiences and particularly under-served populations. She is on the board of directors for The Mental Health Association in Forsyth County, North Carolina chapter of American Foundation for Suicide Prevention, and LEAD Girls of NC. Dr. Dennis is faculty and the creator and Coordinator of the Criminal Studies program in the Department of Sociology and Criminal Studies at Salem College in Winston-Salem, NC. She can be contacted: www.kimyandennis.com ; kimya@kimyandennis.com